What the heck is PGAD?!?!
PGAD stands for Persistent Genital Arousal Disorder. Still confused? Let’s do a deep dive into this. In 2020, a new society report in the Journal of Sexual Medicine was published by the International Society for the Study of Women’s Sexual Health. This report provides an improved understanding of this condition and guidance for evidence-based management. Spoiler Alert: it recommends the use of a personalized, biopsychosocial approach for diagnosis and treatment.
Here’s what you need to know:
PGAD is now referred to as PGAD/GPD, which stands for Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia. This term is more inclusionary and allows a greater number of symptoms to be recognized with this condition.
Before we continue, a quick review: What is “dysesthesia”?
“Pruritus (severe itching), burning, tingling, stinging, anesthesia, hypoesthesia, tickling, crawling, cold sensation, or even pain--without a primary cutaneous condition in a well-defined location that is often caused by nerve trauma, impingement, or irritation.”
So, not just “arousal” but other unwanted sensory experiences.
PGAD/GPD is poorly understood, lacking in quality research, and is not “rare”, presenting in 0.6-3% of the population.
Symptoms of this condition may also be associated with:
Partial or no resolution or worsening of symptoms with sexual activity
Altered orgasm quality in a negative way
Worsening symptoms with certain postures, movements, sounds, stress, anxiety
There are psychological contributing factors and comorbidities found in these individuals:
pre-existing difficulties with mood, anxiety, and stress
past sexual or emotional abuse or trauma
depressive symptoms/suicidality
catastrophizing and hypervigilance of symptoms
obsessive-compulsive symptoms
sexually conservative beliefs
greater neuroticism and lower openness personality traits
relationship issues
What is the best way to diagnose and treat this condition? Biopsychosocial approach!
Diagnosis
Take a good history! Detail symptoms in regards to medical history and psychosocial factors - history of onset, timeline, medications, family history, abuse or trauma, emotions, support system.
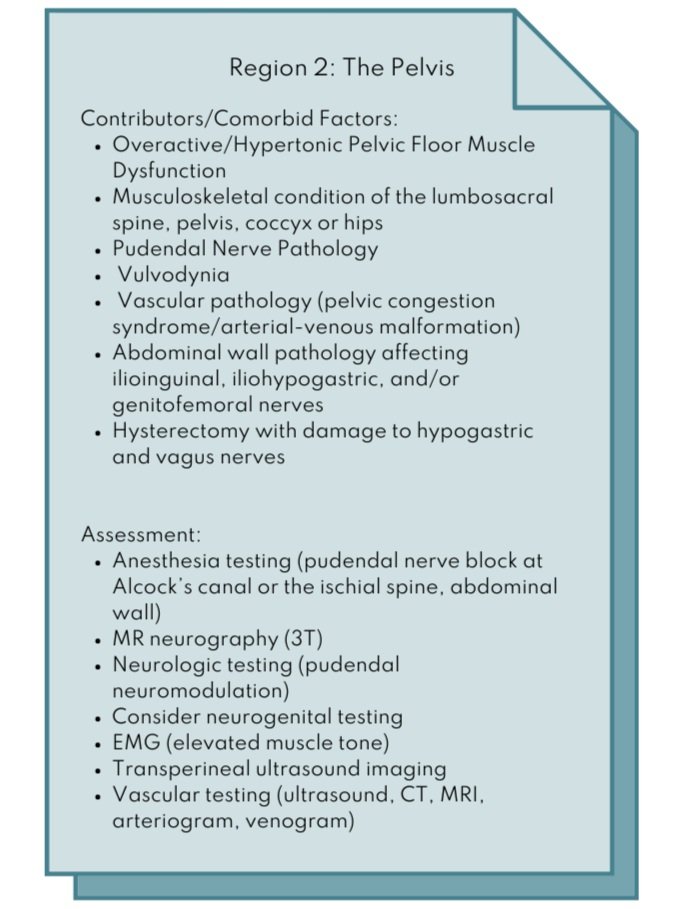
PGAD/GPD symptoms are caused by sensory hyperactivity originating in any of the 5 regions. Localizing the region of origin causing the symptoms is key for optimal treatment.
Physical exam: begin with a detailed assessment from distal to proximal, starting with Regions 1 and 2 due to greater accessibility to these areas.
Treatment
Referral to a medical specialist in sexual health for assessment/testing, medical treatments such as medications, injections, procedures, and referral for other specialists and complementary interventions
Psychological interventions
Alternative medicine: yoga, acupuncture, hypnotherapy, etc.
Pelvic Floor Physical Therapy - standard for those with overactive pelvic floor dysfunction and pudendal neuropathyPelvic floor physical therapy involves:
Patient education - teaching patients to initially avoid/modify/pace triggering activities or positions with a gradual progressive increase
Introduce exercise and activity to reduce symptoms (walking, breathing, relaxation exercises) and self-management tools/modalities
Manual therapy - myofascial release, deep tissue mobilization, trigger point release
Therapeutic exercise: relaxation/lengthening of overactive pelvic floor muscles, improving impairments in strength, stability, endurance
Neuromuscular re-education: active or passive (dry needling)
Possible treatment for chronic constipation and straining
Trigger point injections, suppositories (valium and/or baclofen), and pelvic floor muscle injections of Botox can all compliment PFPT
To find mental health providers who specialize and are certified in sexual health, go to The American Association of Sexual Educators, Counselors, and Therapists.
In conclusion, PGAD/GPD is a complex problem that requires a team of providers to assess and treat the underlying dysfunctions. It is our job, as part of our pelvic health specialty, to guide individuals to providers who can offer the greatest benefit. Consider using the directory of the International Society for the Study of Women’s Sexual Health to locate sexual medicine providers in your area.
Are you looking for a pelvic floor PT to work with for your vulvar issues? If you live in the greater Minneapolis, Minnesota area, my clinic is in Edina, MN. Let’s work together to create an action plan to overcome your pelvic health issues and reach your goals.
Goldstein I, Komisaruk BR, Pukall CF, et al. International Society for the Study of Women’s Sexual Health (ISSWSH) Review of Epidemiology and Pathophysiology, and a Consensus Nomenclature and Process of Care for the Management of Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia (PGAD/GPD). J. Sex Med 2021;18:665-697.
Disclaimer: These self-care suggestions are for general use only and are not intended to be used as medical advice, diagnosis, or treatment. Refer to your medical provider for all questions and concerns regarding your individual care.
Did you enjoy this post? Whether you're a newbie or a pelvic pro, join the community to stay up to date with the latest and greatest in pelvic health!